The microbiota, from discovery to discovery
Until recently, no one imagined that the microorganisms in our gut could play an important role in our health. Today, scientists are highlighting the links with many diseases, paving the way for a real revolution in our approach to health.
Published on 06 October 2022
1940s The right method
The story began in the 1940s in the United States with a microbiology researcher, Robert Hungate, who developed a technique –still in use today– for cultivating bacteria from the rumen (the first digestive compartment of ruminants) of cattle, whose particularity is that they only grow in oxygen-free environments (strict anaerobic bacteria). Until then, it was impossible to characterise them because it was impossible to cultivate them. With this method, the hitherto unknown world of anaerobic micro-organisms that reside in the digestive ecosystems of animals and humans was opened to knowledge.
The question was clear: how do the microorganisms in the rumen of cattle participate in the digestion of fibres?
1980s Microbiota and animal production

At INRA, the first work on what was then called “the rumen flora of animals” was carried out in 1980 in the microbiology laboratory of the Theix centre (Clermont-Ferrand). The question was clear: how do the microorganisms in the rumen of cattle participate in the digestion of fibre, the cellulolysis, a major function that was beginning to be described at the molecular and cellular level?
“We were the forerunners in the description of anaerobic fungi discovered in the rumen of herbivores, and then we were the first to demonstrate that protozoa produced enzymes that degraded fibres in the rumen”, recalls Évelyne Forano,
research director at the MEDIS joint research unit. At the same time, antibiotics were being used as growth promoters in livestock farming. Researchers therefore became interested in understanding the mechanisms of action of these antibiotics administered at low doses, but sufficient to limit the pathogen load,… in order to then do without them to meet a regulatory requirement! One of the approaches envisaged was to enrich the microbiota of farmed animals by feeding them live microorganisms, called probiotics, to reinforce the barrier effect against pathogens; this is how studies on probiotics used in the field of ruminant nutrition began.
What happened to the gut flora?
We all have in mind the term gut flora to represent the microorganisms of our digestive system. This term disappeared in the early 1990s when Carl Woese proposed a new classification of living organisms. Until then, bacteria were considered to be plants, and it was only natural that micro-organisms were referred to as flora. But in 1990, Woese's new classification, distinguishing between bacteria, eukaryotes (including plants) and archaea, made the term “flora” for bacteria... inappropriate! It was then replaced by “the microbiota”.
1990s From animal to human

Impossible for scientists not to wonder about the human equivalent, known at the time as the gut flora. “We applied all the methodologies acquired on animal microbiota to the study of human microbiota, explains Évelyne Forano, and this accompanied the development of studies on human nutrition at INRA, following the creation of the scientific division NASA (Nutrition, Food and Food Safety).”
Over the same period, new molecular techniques, including DNA sequencing, were being developed. A true revolution for science.
The contribution of DNA sequencing
Stanislav Dusko Ehrlich, then director of research at the Microbial Genetics Unit in Jouy-en-Josas, seized on these new technologies to gain a better –and much faster– understanding of the roles of lactic acid bacteria. Convinced that knowledge of the genome would make it possible to explain the biology of bacteria (growth, reproduction, feeding), Stanislav Dusko Ehrlich embarked on sequencing the genome of Bacillus subtilis, the complete sequence of which would be published in Nature in 1997. Numerous studies then ensued to characterise the animal and human microbiota by analysing its DNA: “Thanks to DNA analysis, we can characterise the entire system, including bacteria that are difficult to cultivate (because they are sensitive to oxygen), which represent 70% of the microbiota”, explains Joël Doré, Research Director at the Micalis1 Institute and Scientific Director of the MetaGenoPolis unit.
1. Joint research unit associating INRAE, AgroParisTech and the University of Paris-Saclay.
2000s What is the use of the microbiota?

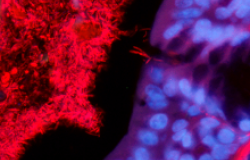
While DNA sequencing had made it possible to characterise the microorganisms of the microbiota, it remained to be seen –and understood in detail– what it is used for and how it functions. A little anecdote on great research: “Joël and I were talking in a café on rue Claude-Bernard, the father of modern biology: you can’t make this up!” recalls Hervé Blotot, then a biologist at the Micalis Institute. What can a microbiologist and a cell biologist have to say to each other? “[…] We told ourselves that we had to study the dialogue between bacteria and cells!” The circle was complete, and a new approach was born, which consisted in analysing the interactions between the cells of our body and the microorganisms of our microbiota: functional metagenomics! The two researchers, with their teams from the Micalis Institute, then went on to develop a tool (MetaFun, a high-throughput cloning/phenotyping platform) allowing them to incorporate pieces of the genomes of intestinal microbes into the Escherichia coli bacterium. They obtained thousands of clones that they put in contact with human cells capable of emitting light or colour when a dialogue is established. This makes it then possible to find out which microbial gene is responsible for the functional changes observed in human cells.
Microbiota and health
By combining quantitative and functional metagenomic techniques, scientists are opening up new research perspectives: understanding the link between microbiota and health. In quantitative metagenomics, the microbiota of patients and of healthy subjects are compared, obtaining a characterisation typical of the “sick microbiota”; this allows to make a possible diagnosis and sometimes even to predict the occurrence of the disease or its aggravation in a patient.
In functional metagenomics, the aim is to identify the mechanisms of interaction between cells and microorganisms, as well as their consequences, assumed to be responsible for the disease. The aim is then, among other things, to develop drugs to re-establish a good functional microbiota-host dialogue, and subsequently the patient's state of health.
Another method for establishing the link between microbiota and pathologies is to use axenic animals, which are raised in a sterile environment and therefore have no microbiota. By implanting them with the microbiota of a sick patient, one sometimes observes that they in turn develop the symptoms of the disease. Naturally, scientists first turned their attention to inflammatory bowel diseases, including Crohn's disease, for which a direct link with the state of the microbiota was established in 2006.
2010s The decoding of the microbiota genome, a major advance for medicine
Almost 2,000 species of microorganisms have been identified. Each human being is home to about 300.
If there was a major step forward in the understanding of the microbiota, it was definitely this one. “Our other genome”, was the title of the prestigious journal Nature in March 2010. After several years of work, and as part of the MetaHIT project coordinated by Stanislav Dusko Ehrlich, the genome of billions of microorganisms has been deciphered! An initial catalogue of 3.3 million genes was published in 2010, completed in 2014 to reach 10 million genes. The question that then drove the scientific community: do we all have the same microbiota? The hypothesis was that there is an “average human microbiota” with a relatively identical composition of microorganisms.
Wonderous world of science, “we had two surprises with this work, recalls Joël Doré enthusiastically, the first is that there is no such thing as an average microbiota, but at least three major types of microbiota!” Or rather enterotypes, i.e. three ecological organisations each dominated by a particular bacterial genus: Bacteroides, Ruminococcus and Prevotella. “The second surprise was that we observed rich and poor microbiota in terms of gene diversity, and therefore of microorganisms.” As you might expect, the next step in this train of thought was: is there a link between enterotypes, the richness of the microbiota and the onset of chronic diseases? Joël Doré's answer is clear: “Yes, a microbiota that is poor and of the Bacteroides enterotype is associated with a higher risk of cardiometabolic diseases. These are the first results, and there is still a long way to go!” In parallel with these major discoveries, links between microbiota and various pathologies were continuously being brought to light: in 2012, scientists established a link between microbiota and type 2 diabetes, in 2013 with obesity, in 2014 with cirrhosis and with fatty liver syndrome. In 2018, scientists discovered that certain bacteria in the microbiota could facilitate cancer treatments. Even more surprisingly, links were established between the microbiota and neurodegenerative diseases (multiple sclerosis, Parkinson's and Alzheimer's) as well as neuropsychiatric disorders (autism, bipolarity, schizophrenia, depression). Although the link between the state of the microbiota and this type of pathology was observed in animals in the early 1980s, the mechanisms governing this association have only recently been discovered: an alteration in the microbiota leads to inflammation in the intestine, which favours permeability of the blood-brain barrier. The role of the barrier is to prevent the passage of potentially toxic substances or pathogens into the brain and spinal cord. This permeability leads to inflammation in the brain, which is thought to promote the development of neurodegenerative and neuropsychiatric diseases.
In 2017, a strong link between the microbiota and autism spectrum disorders was confirmed. Research is ongoing within the framework of the European Gemma project (2019-2025) to study the role of the gut microbiota in these disorders. Also in the 2010s, MetaGenoPolis was created. It is a pre-industrial demonstrator with state-of-the-art equipment to go further and faster in understanding the microbiota and to develop innovations for society.
A life in symbiosis
As discoveries were made about the links between health and the microbiota, a new way of looking at them emerged. It is not enough to act directly on the microbiota, but rather to take into account the “microbiota and host” as a whole and therefore to also care for its environment (the host), our body. The results showed that it is indeed the way we take care of ourselves that allows our microbiota to be well-balanced and, in turn, contributes to our good health.
At this point, the concept of symbiosis between the microbiota and the host gained a foothold and gave rise to the concept of dysbiosis, which occurs when the symbiosis is altered! Dysbiosis can occur in the event of oxidative stress, a decrease in bacterial diversity, an increase in the permeability of the intestinal barrier or an inflammatory state, all of which explain the link with the many pathologies mentioned above. Once the balance is altered, these parameters maintain a vicious circle creating a context favourable to certain chronic diseases that are at present incurable.
Transfer of microbiota
If the links between microbiota and certain pathologies are so obvious, why not transfer a healthy microbiota to a sick individual in order to treat them? This is the idea that led to the creation of the start-up MaaT Pharma in 2014, of which Joël Doré is still the scientific advisor. INRA and MaaT Pharma then jointly developed a microbiota transfer technique that consisted of administering a suspension of stool from healthy donors into the digestive system of a sick recipient in order to restore the richness of his or her microbiota and provide a health benefit. The results obtained in 2016 are promising. Although there are still risks in transferring microorganisms from one individual to another, this work opens up new approaches to the treatment of severe diseases for which medicine sometimes has no solution left.
Maat Pharma, the start-up developing new therapies thanks to the microbiota
Created in 2014 based on INRA's know-how and more broadly on the work of Micalis and MetaGenoPolis, the start-up MaaT Pharma develops and standardises technologies to secure the therapeutic use of microbiota transfer. Its initial work consisted of developing a process for conditioning intestinal content, making it possible to freeze-dry it in order to encapsulate it. Today, the research centres on the transfer of healthy microbiota via these capsules for therapeutic purposes in the treatment of cancer. Indeed, this transferred microbiota makes it possible to rebuild the host-microbiota symbiosis and thus to restore immune homeostasis.

In 2016, their clinical trials made it possible, thanks to the transfer of microbiota, to rebuild a normal symbiosis in 90% of patients with acute myeloid leukaemia who had undergone chemotherapy. In 2021, they showed that microbiota transfer improves the survival rate of patients with graft-versus-host disease, a severe complication that sometimes occurs following bone marrow transplantation in the treatment of blood cancer. Currently, they are developing drug candidates that exploit the potential of microbial ecosystems throughout the care path of cancer patients.
2020s The revival of preventive medicine

Work on host/microbiota symbiosis is continuing and expanding. A new project, The French Gut, began in September 2022 and aims to characterise the microbiota of the French population by collecting stool samples from 100,000 volunteers. For Joël Doré, this work offers in addition to new research perspectives a new way of thinking about health, moving towards preventive nutrition and using the microbiota as a lever.
The French Gut : mapping the microbiota of the French

In Septembre 2022, INRAE launched an ambitious project, The French Gut, to gain further knowledge of the microbiota and its links with health. The aim is to collect the stools of 100,000 volunteers as well as the associated nutritional and clinical data, and to analyse them in order to better understand what a healthy gut microbiota is and what alterations are observed in the case of disease. Led by INRAE, The French Gut project is conducted in partnership with public and private institutions involved in microbiota knowledge. The ultimate goal is to open the way to innovative therapies to treat chronic diseases (such as diabetes, obesity and cancer) and neurodevelopmental disorders. The French Gut is part of the worldwide Million Microbiome of Humans Project (MMHP) which aims to analyse one million microbial samples from the intestines, mouth, skin and reproductive system.
Diagnosis and medication
As far as diagnosis is concerned, one day it will undoubtedly be possible to carry out a microbiota analysis in the same way as a blood test to assess the state of the symbiosis and help in the management of pathologies. Regarding medication: “According to our initial results, acting simultaneously on the microbiota, the permeability of the intestinal barrier, inflammation and oxidative stress could be just as effective as standard drugs”, explains Joël Doré. Indeed, an experiment on mice shows that a combination of a probiotic (which protects the intestinal barrier and has anti-inflammatory properties), glutamine (an amino acid that also protects the intestinal barrier) and curcumin (a polyphenol, anti-inflammatory and antioxidant), acts on the four factors of dysbiosis and gives results that are just as effective in treating depression as the antidepressant clomipramine, but without the side effects. In other words, the microbiota revolution has only just begun!
Microbiota and Covid-19
3 questions to Philippe Langella, Director of Research at the Micalis Institute
Is there a link between Covid and microbiota? Analyses of the gut microbiota of patients with Covid-19 show a dysbiosis, i.e. an imbalance of the microbiota, which is characterised by a decrease in bacteria with anti-inflammatory activity, a decrease that is all the more significant the more severe the form of Covid-19.
Is there any way to avoid such dysbiosis in the case of Covid? For many years, our laboratory has been developing prevention and therapeutic strategies based on new-generation probiotic bacteria to combat intestinal inflammation. The idea is to evaluate whether they could be used additionally in Covid patients to avoid the intestinal damage that is observed in 20% of them.
What are new generation probiotics? Probiotics are live microorganisms that are ingested with the aim of restoring or maintaining our host-microbiota symbiosis. Until now, the probiotics used were either derived from the consumption of fermented foods or from food supplements, but always obtained from natural ferments. The new generation of probiotics is now directly derived from the gut microbiota.
The microorganisms, a vast world
The gut microbiota is not the only one in our body, but to date it is the most documented. We have a microbiota on the skin, in the mouth, the vagina, the lungs, the eye and so on. All these microorganisms form a microbiome which itself forms, together with its host, a holobiont. But there are also microorganisms in our environment, in the earth, in the air, in plants, on and in animals.
All these microbiomes can interact and these interactions, on a more global scale, are still a little-known area of research. One example is antibiotic resistance. By dint of using antibiotics for our health and that of animals, we are encouraging the emergence of antibiotic-resistant bacteria. This is becoming a global problem affecting our health, that of animals and of the environment. In 2020, INRAE launched a research metaprogramme called HOLOFLUX, “Holobionts and microbial flux within agrifood systems”.
Its objective is to gain a better understanding, on the one hand, of the interactions within holobionts (between microbiota and hosts) and on the other hand, of the flows of microorganisms between holobionts and the agrifood system as a whole. This knowledge would make it possible to use them as levers for performance, sustainability and the preservation of human, animal and plant health.
Humans, animals and plants are all holobionts. This concept is now underpinning more and more scientific projects, which range from the study of environmental, animal or plant ecosystems to that of immunity, nutrition and human health.
-
Elodie Regnier
Author / Translated by Alessandra Riva